Uncovering How Posterior Tongue Tie Affects Speech, Breathing, and Jaw Health

I’ve dealt with chronic teeth grinding (bruxism) and jaw pain (temporomandibular joint disorder, or TMJD) for most of my life. (Read here about how it increased my empathy!) It wasn’t until I was 48 that I learned a surprising possible contributor: a mild, previously undiagnosed, posterior tongue tie.
What is posterior tongue tie?
A posterior tongue tie is further back under the tongue than we traditionally think of a tongue tie. It is not as easily seen and was previously thought to not have much of an impact on an individual’s health or well-being. I know I’d never heard of it, even as an SLP.
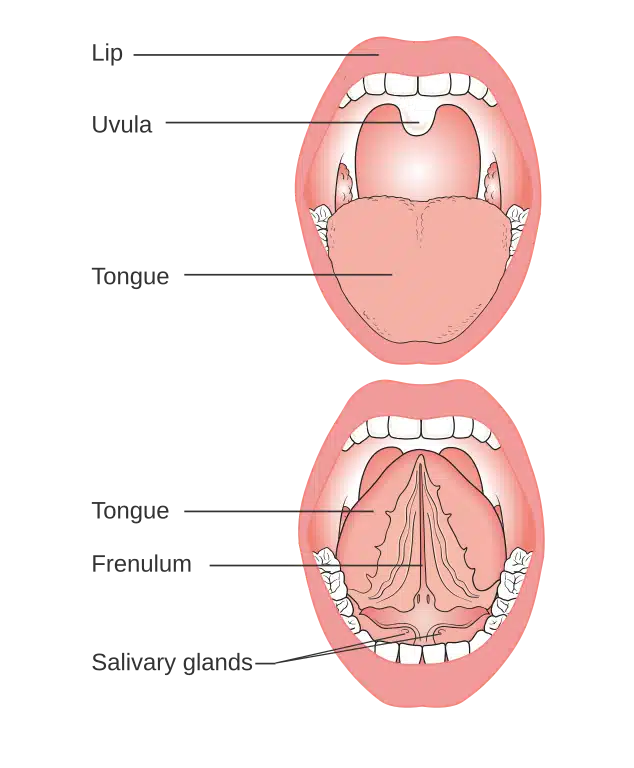
Apparently, I had been compensating for the difficulty in raising my tongue. I was using other parts of my mouth in ways they weren’t meant to be used. For example, while I could move my tongue tip to the spot just behind my teeth, even with my mouth open. However, when I did so, my tongue pulled all the fascia in the floor of my mouth, like the salivary glands, with it. This made the movement much more effortful.
I could definitely feel the pull when I tried to open wide and touch my tongue tip to the top. To stick my tongue outside of my mouth, especially to the side, I had to compensate. I was using my jaw and lips to increase the range of motion. To swallow, my tongue thrust forward, compensating for the decreased mobility of the back of my tongue.
I share my experience to raise awareness about the complexities of tongue tie. My hope is to encourage others to explore potential connections between speech, swallowing, and other oral health issues with this often-overlooked condition. This information can empower individuals to seek appropriate evaluation and treatment.
What exactly is Tongue Tie?

Traditionally, we think of tongue tie (ankyloglossia) as a simple condition. It involves a short, tight band of vertical tissue running from the bottom of the tongue to the floor of the mouth (the lingual frenulum), which restricts tongue movement. You can see an example of the traditional concept in the picture on the left.
But the reality is much more nuanced. Current research is beginning to recognize that tongue tie can present in various forms. This includes subtle limitations and attachments further back in the tongue (posterior tongue tie), which may not be immediately apparent.
For years, the focus was on severe limitations, primarily impacting breastfeeding. When I was in graduate school (a quarter of a century ago!), tongue tie was briefly mentioned. At that time, it was considered to impact an individual only if the tip of the tongue could not reach the alveolar ridge. Basically, if the child could breastfeed and say /t/ or /th/, it was considered sufficient. Which explains why I was first identified as having a tongue tie at 48!
The recognition and understanding of tongue tie are continuously expanding. As we delve deeper, its potential impact on overall health is also becoming clearer. This is an evolving field, with ongoing research to refine assessment and classification methods. Currently, there is no single, universally accepted evaluation protocol. This can sometimes lead to varying interpretations and approaches among healthcare professionals.
However, emerging evidence suggests that even subtle restrictions can have significant, often overlooked, consequences.
New tongue tie assessment protocol
- Length between tongue tip and the attachment of the frenum to the tongue (Kotlow Free Tongue Measurement)
- Difference between maximum opening of mouth and maximum opening with tongue tip to just behind top teeth
- Difference between maximum opening of mouth and maximum opening with tongue suctioned to roof of mouth
- Compensations – floor of mouth, jaw, lips, neck
- Tension – present or absent in mouth, jaw, neck, etc.
It is the presence of the compensations and tension more than the measurements that are more indicative of a problem with the tongue tie, especially in adults. And yet, those are the most difficult to consistently “measure,” especially between professionals.
How does posterior tongue tie affect feeding and swallowing?
A posterior tongue tie affects the mid and back of the tongue. It can interfere with the proper movement of the tongue and cause issues with proper feeding and swallowing. Some experts even argue that a posterior tongue tie is more detrimental than an anterior!
Babies:

- creating the seal needed for breastfeeding
- fussy feeding
- choking, coughing, gurgle sound
- inefficient sucking, can lead to increased air intake during feeding causing excessive spitting up
- Feeding fatigue
- Cracked, bleeding, or severely bruised nipples
Children (and adults):
- poor chewing movement and control of food bolus (clump), which can cause food spillage and/or food left in pockets of mouth
- Poor movement of food bolus to the back of the mouth for swallowing
- Increased risk of choking or gagging
- may result in reluctance to try new textures
The Lesser-Known Impacts of Tongue-Tie
Feeding and swallowing difficulties are well-known to be symptoms of tongue tie in babies. However, the impact of tongue tie can extend far beyond infancy and feeding. It can affect various aspects of oral health and well-being.
Research on the long-term consequences of tongue tie in adults is still ongoing. Furthermore, there is no standardized assessment and classification system for tongue tie, especially posterior. This presents a challenge in consistently identifying and understanding its impact across different individuals.
Oral Motor and Articulation Challenges
- Oral Motor Challenges: Restricted tongue movement can affect oral motor skills crucial for chewing, swallowing, and even breathing. This may present as difficulty licking lips, blowing bubbles, or clicking the tongue.
- Speech (Articulation) Difficulties: Because posterior tongue tie is often overlooked, it may be a hidden contributor for children who have trouble with back sounds, such as /k,g,r,sh/.
Dental and Jaw Health

- Dental Issues: Some studies suggest that tongue tie and the resulting poor oral posture can contribute to dental problems. These include crowding, misalignment, and even underbite or overbite. Tongue positioning has also been suggested to affect the way the upper and lower jaws grow and develop. This can occur because the tongue plays a crucial role in proper tooth and jaw development and alignment.
- Jaw Pain and Dysfunction: My experience highlights a potential link between undiagnosed tongue tie and TMJ problems. Symptoms include as jaw pain, ear pain, clicking, locking, and limited jaw movement.
- Bruxism (tooth grinding): Studies suggest abnormal tongue posture and function may exacerbate, or even cause, bruxism. This could potentially contribute to TMJD. A current theory is that some, if not all, bruxism arises from the jaw’s attempt to find a comfortable resting position. Proper tongue posture can naturally provide this comfortable resting position for the jaw. The exact relationship between tongue tie, tongue posture and bruxism is still under investigation.
- Breathing, Snoring, and Sleep Apnea: While tongue tie can sometimes contribute to sleep-disordered breathing, such as upper airway resistance syndrome (UARS), it’s not a direct cause of sleep apnea. However, good resting oral posture, often compromised by tongue tie, is crucial for healthy breathing. This can lead to mouth breathing, impacting oxygen intake among other things.
Breathing and Sleep Issues

- Mouth Breathing: Good resting oral posture is important for healthy breathing. However, posterior tongue tie can compromise oral posture and can contribute to mouth breathing. Studies have shown that mouth breathing may impact oxygen intake, among other things.
- Snoring: Many people with tongue tie may also have a longer velum (uvula), or soft palate. This soft tissue is likely stretched to compensate for restricted posterior tongue movement, which can increase the risk of snoring.
- Regular snoring, in both children and adults, should be evaluated by a medical professional.
- Snoring can significantly disrupt sleep quality, leading to daytime fatigue, difficulty concentrating, and an increased risk of accidents.
- Furthermore, chronic snoring can increase the risk of serious health problems, including high blood pressure, heart disease, stroke, and type 2 diabetes.
- Sleep Apnea: While tongue tie can, in some cases, contribute to sleep-disordered breathing, such as upper airway resistance syndrome (UARS), it’s not a direct cause of sleep apnea.
The Importance of Early Recognition
Early identification and intervention are crucial. For infants, addressing tongue tie can improve breastfeeding, speech development, and overall oral health. However, it’s important to remember that tongue tie can still be addressed in adults.
My personal journey has been eye-opening. While I may not be able to completely reverse the effects of years of undiagnosed tongue tie, I’m exploring treatment options. My goal is to improve my oral function and overall well-being.
Treatment team can include:

- Pediatrician or General Practitioner: Often the first point of contact for tongue-tie concerns, they can conduct initial assessments. They also refer to other specialists as needed.
- Orofacial Myofunctional therapist – Most often a specially certified dental tech or SLP, they specialize in correcting improper function of the oral and facial muscles. This includes tongue posture and movement.
- Otolaryngologist (ENT) – Specializes in disorders of the ear, nose, and throat. They can diagnose and treat tongue-tie, including performing surgical procedures.
- Dentist – an assess tongue-tie’s impact on oral health, including dental development and alignment. They may also perform tongue-tie release procedures (frenectomy).
- Physical therapist (PT) – Tongue-tie can sometimes contribute to postural imbalances. PT can help address these issues, such as forward head posture, which can impact oral function.
- Lactation Consultant – Assists with breastfeeding challenges related to tongue-tie, providing guidance to both mother and infant.
- Speech-Language Pathologist (SLP) – Evaluates and treats speech, language, and feeding/swallowing difficulties related to tongue-tie. They can also provide oral motor exercises and therapy to improve tongue function.
A Call to Awareness
This experience has reinforced the importance of:

- Broadening our understanding of tongue tie.
- Early identification and intervention.
- Considering tongue tie as a potential factor in a wider range of oral health and developmental issues.
- More research on classifying tongue tie and how it impacts daily life.
If you have concerns about your child’s speech, feeding, or oral motor skills, consult a qualified healthcare professional. This includes a pediatrician, dentist, or speech-language pathologist. The same applies if you experience any of the issues mentioned above.
Resources:
- Tongue Tie
- Tongue Tie Images, including TRMR-TIP and TRMR-LPS Classifications, and links to information
- How tongue mobility changes face and jaw development
- Correct Tongue Posture: Why correct tongue posture affects your whole face (including your teeth!)
- “Do I Have A Tongue-Tie?” – 5 dimensions of tongue-tie assessment, Dr. Zaghi – The Breathe Course (mostly for professionals, very in-depth)
- Pediatric Sleep-Disordered Breathing and Obstructive Sleep Apnea: The Role of the Speech-Language Pathologist
- Tongue Tie, Airway, & TMJD – Priya Mistry, DDS (the TMJ doc) #tonguetie #airway #tmjd
- What is a Tongue Tie? – Priya Mistry, DDS (the TMJ doc) #tonguetie #nursing #tonguetied
I hope this article provides valuable information and encourages further discussion about this under-taught and often-overlooked condition.
Social Media Icons: designed by rawpixel.com – Freepik.com